Breast reconstruction can be classified into two categories: implant reconstruction and flap reconstruction (using your own tissue for breast reconstruction instead of implants). 80-90% of women opt for implant reconstruction because flap reconstruction is a much more invasive type of surgery involving both the breast and the site where the flap is taken from that requires a much longer procedure time and hospitalization, as well as extensive recovery after surgery.
The main benefit of implant-based reconstruction is that no large additional scars outside of the breast are needed and the post-operative recovery is often easier, with a typical two- to four-week recovery period.
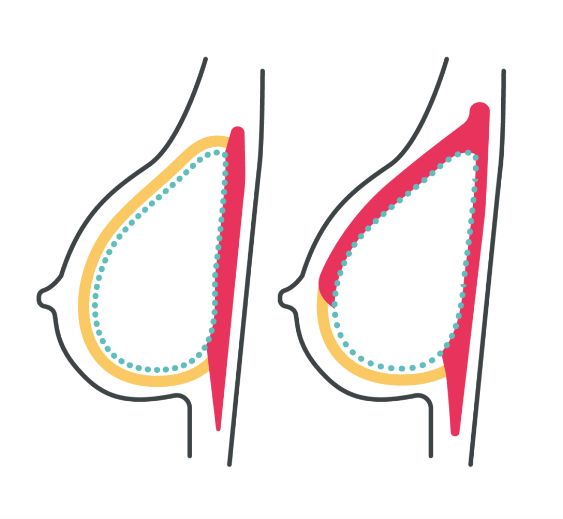
Implant-based reconstruction for mastectomy can be done in either one stage, where a permanent implant is placed at the time of mastectomy, or in two stages, where a temporary implant called an expander is placed at the first stage and switched to a permanent implant at the second stage. The decision on which approach to use is based on pre-mastectomy breast size and shape, patient goals, and intra-operative assessment following mastectomy. Implant-based reconstruction may also include fat grafting at the second stage of reconstruction in order to help give the most natural appearance of the breast following reconstruction.