With over 16 years of experience as a plastic, reconstructive, and peripheral nerve surgeon, I have seen many aspects of this diverse and interesting field of medicine. One particular area of passion and commitment is my focus on sensation-preserving mastectomy, a field I have been fortunate to develop and collaborate on with my wife Anne, herself an equally accomplished & talented plastic, reconstructive and breast surgeon. Our partnership, both professionally and personally, has allowed us to develop a unique approach to breast surgery that truly sets us apart.
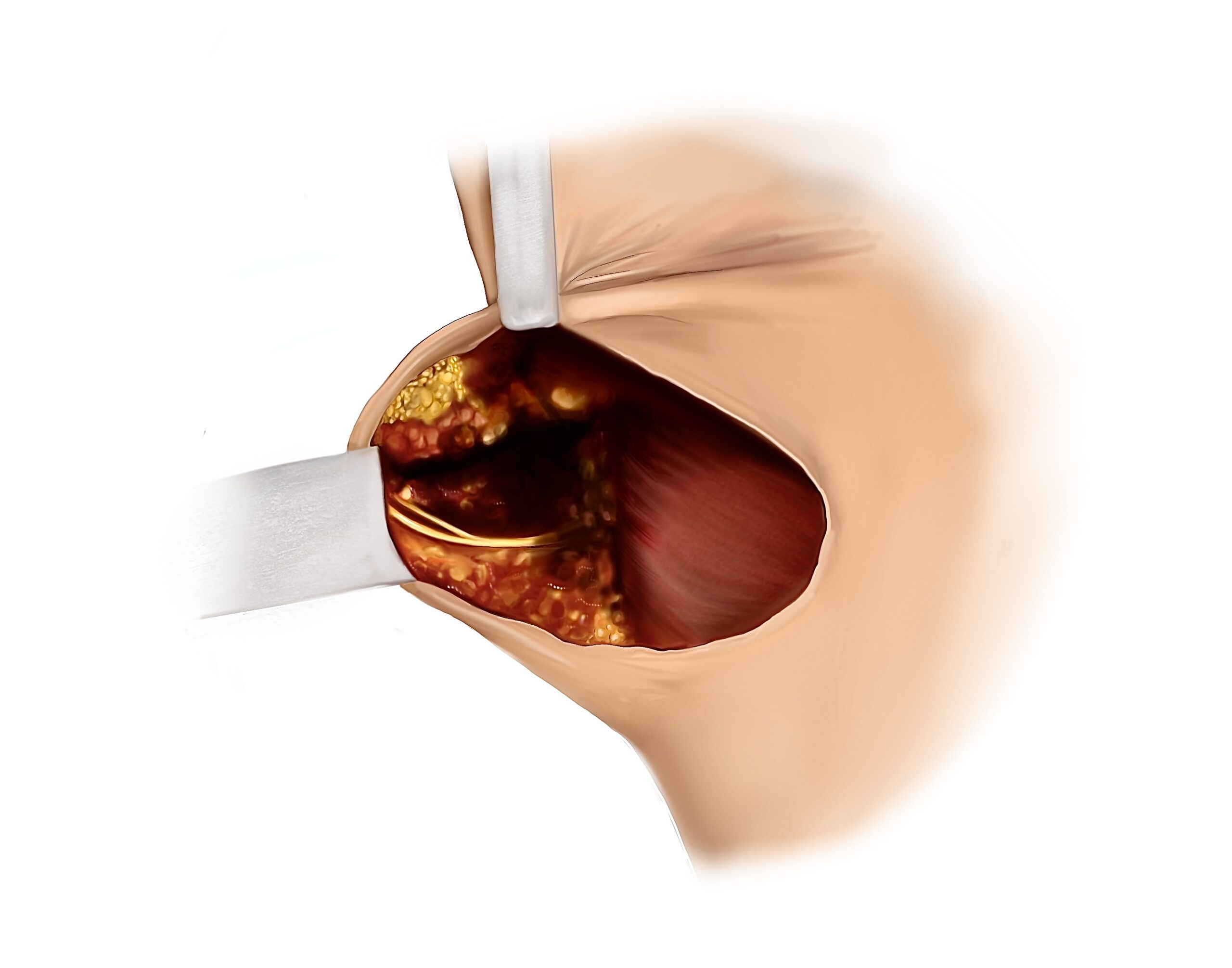
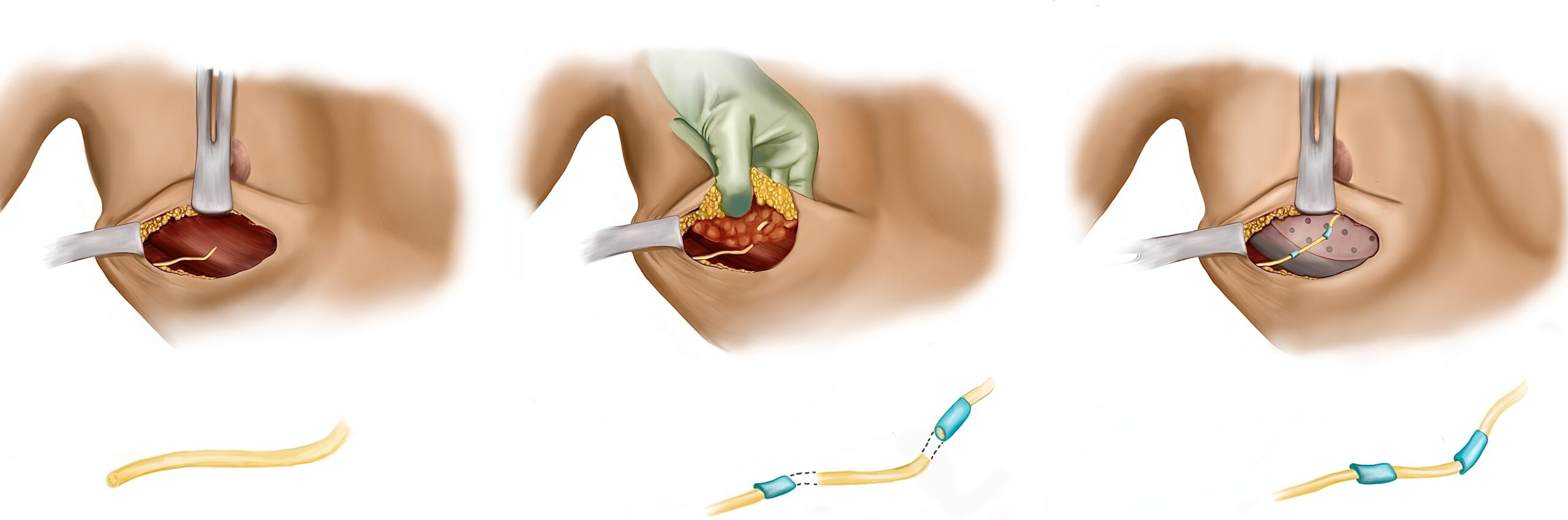
Following a mastectomy and most types of reconstruction, most women are completely numb because remarkably, little attention is paid to the nerves providing sensation to this important area of the body. Historically, this lack of sensation following a mastectomy is the aspect of their medical journey with which women are most dissatisfied, often leading to long-term, negative psychological and emotional effects. This lack of sensation is also important from a functional and safety standpoint because loss of protective sensibility can result in undetected wounds to the area, potentially having a severe and detrimental impact on any underlying reconstruction.